Our society struggles with the issue of physician assisted suicide, or assisting a patient to die. Dr. Kevorkian went to prison, and after spending that time there never again wanted to rally people to his cause- prison for Kevorkian was a place he didn’t want to return to, and certainly not worth advancing that cause.
But in California, there is a lawsuit seeking to exempt physicians who seek to help terminally ill patients end their lives. Some from California are going North to Oregon where it is legal for a doctor to assist a patient to end their life.
For some, it is a cavalier discussion, saying things like, “We don’t allow our dogs to suffer, why do we allow people to suffer?”
Others hear about the personal decisions of doctors, who chose not to have treatment for advanced cancer, get their affairs in order, and choose to die “peacefully.”
But it is never that simple.
The obvious questions:
Do we know for certain that someone is “terminal?”
Yes- often we do. We are better at knowing that someone will not survive a disease than we are at predicting who might die from an intervention of the disease.
Could this power be abused – with elderly, or demented, or people that we just don’t want to take care of?
Yes- it can be abused.
What about the pressure to end the lives of those who have high costs of treatment, or if insurance refuses to pay for their care?
Yes- it can be abused.
So let me tell you the story of my brother, Jimmy.

Jimmy – just before being diagnosed with Hodgkin’s disease – his first bout with cancer
When he was 18 years old, in the Navy, he found a lump on his neck. We joked it was some strange disease he picked up in SouthEast Asia (it was during the Viet Nam War). But the lump was Hodgkin’s disease. He was sent south, where he underwent exploratory surgery and the Hodgkin’s was found above and below of the diaphragm. His chance of survival was miniscule. But he was in the Navy, and at the Naval base they had signed on with Dr. Kaplan of Stanford, to participate in a trial of radiation vs radiation and chemotherapy alone. It was a “hail Mary pass,” a last ditch effort. Jimmy volunteered.
He was randomized in the radiation only group. It was a miserable time. The letters my parents in Alaska received were heart wrenching, as my brother was tired, wanted to give up, vomited. But he sustained. And he won – one of the few lucky who underwent an experimental therapy on a cancer that was considered fatal.
He left the Navy on a medical exemption – and came home to Alaska. Jimmy was a popular kid; all of his friends from high school loved him. They gave him the nickname, “the cancer kid.” He met his wife, Bev, they lived together for a few years before they married – she was attracted to this young man that everyone loved, this “cancer kid.”
Sadly, the cure left him unable to have children – and of all people who loved children, Jimmy was one. I remember being in the bathroom where some little kid wanted to go to the bathroom, but the door was closed – no one was inside. Jimmy said, “Just go under the door.” He looked for approval, and Jimmy smiled. The kid, maybe 5, scrambled under the door and relieved himself. Jimmy turned to me and said, “I wish I could have 12 of them.”
Throughout the years Jimmy always kept in touch with his friends, and their kids. He would play with those kids for hours, no matter how tired.
Then he became more tired. He had a major heart attack, stopped smoking, and stopped drinking. Five years later he developed a cough. Multiple xrays, bronchoscopy and there was no clue. A CT scan showed a large metastatic tumore in his liver that was lung cancer. He was told he had, at the most, a few months left to live.
He could not stop coughing – it was disabling. This strong man was now limited to oxygen tubing and sitting by his fireplace. He told his wife to “sell everything,” including his beloved Corvette – he knew the end was near.

With Bev, his future wife
Jimmy and Bev went to talk to the oncologist, the cancer doctor. They thought, and I agreed, that maybe some chemotherapy would reduce the cancer a bit, and make him feel better for a bit – maybe stop the disabling cough.
He had a round of chemotherapy – and he became sick from it- septic. He was placed in the ICU, on a ventilator. Before he was on it he was able to hug his mom, tell her that he loved her- then he was intubated.
Every weekend for three weeks in 2006 I flew between Phoenix and Portland – my good friend told me, “You have the means to go there, so use it, fly there and be with your brother.”
After 18 days it was clear he would not survive. We removed the tube that kept him breathing. My family came, we got Jimmy’s dog into the ICU, thanks to wonderful nurses, and placed the dog on top of him – and after the dog licked his face, Jimmy sat up for a second, then fell back- and died.
One case a highly experimental therapy kept him alive with certain death. In the second case, a low dose of a chemotherapy brought death sooner.
People say that someone dies peacefully – I don’t believe it. I don’t think death is peaceful. I don’t think every cell of your body that cries out for more oxygen or nutrition, is a peaceful way to die. I don’t think there is dignity in death, I think there is just death. That isn’t a popular view, that isn’t a view people want to hear – but it is a view.
I also don’t think there is dignity in “fighting the good fight,” in trying every ounce of chemotherapy to the exclusion of the time left. But that also isn’t a popular view.
This was in Oregon, before the law allowing doctors to “assist” in suicide. Would Jimmy have gone for that? No- he had beaten cancer once, and while he didn’t think he was going to beat it then – he thought, with encouragement from me, and his oncologist, that maybe it would make him feel better.
Some might point that he cost the medical system a lot of money in his last few weeks of life—he did. Some note that the radiation from the Hodgkin’s therapy came back to kill him – it did. But it gave him years.
At his funeral my dad asked people at the service to raise their hands who knew him since Ketchikan – most of the people there knew him, and traveled far to go to it.
Let us not pretend this is an easy discussion – let us not pretend we know what we would do, or that we should have the ability to say what someone should do with their life, or the end of their life.
But here is what this isn’t: this isn’t a discussion for the courts to have. This isn’t a discussion for physician organizations to have. This isn’t something you can impose on another human being.
I’m a doctor – I am bound to relieve suffering. I know the interventions that I give to people will cause them suffering – surgery does that. I know that as the morphine pump goes up the chances are that the terminally ill person will die, and that some have assisted in raising that morphine so someone doesn’t “struggle, “ (a code word for assisting in their death).
I am happy to assist someone in going to Hospice, or having Hospice come to their home. But I cannot honestly tell you what I will do if faced with a terminal disease.
Because of my brother, and his love of children, when I became a father at the age of 53, I named my son after him.
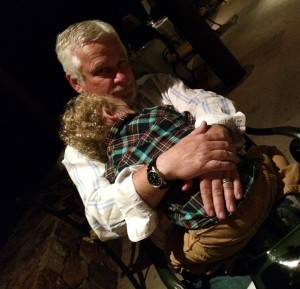
When I hug my son, who is named after my brother- it is like a hug to my brother
